
Osteoarthritis, pain and anti-inflammatory drugs
Partager
Osteoarthritis is one of the most common joint diseases, affecting millions of people worldwide. While there is no miracle cure for this degenerative cartilage disease, many treatments aim to relieve symptoms. Among the most popular are anti-inflammatory drugs, which are widely prescribed to calm pain and reduce inflammation. However, these medications, while effective in the short term, do not address the root causes of the disease and can cause significant side effects.
What is osteoarthritis?
Osteoarthritis is a chronic disease characterized by the progressive wearing away of the cartilage that covers the ends of bones at the joints. Cartilage plays a crucial role in cushioning shock and facilitating smooth movement of joints. However, with age, trauma, excess weight or other factors, this cartilage becomes thinner, cracks or even disappears in some cases, leading to pain, stiffness and loss of mobility.
Symptoms of osteoarthritis
Signs of osteoarthritis vary from person to person, but typical symptoms include:
- Joint pain: often felt after exercise, or sometimes even at rest in advanced stages.
- Stiffness: especially after a period of inactivity, such as in the morning upon waking.
- Reduced mobility : Joints become less flexible and move with difficulty.
- Crepitations : Rubbing or cracking noises when moving.
- Swelling : The joint may become swollen, especially due to inflammation.
Although these symptoms can occur in any joint, osteoarthritis primarily affects the knees, hips, hands and spine.
Anti-inflammatories: a quick but temporary solution
Anti-inflammatory drugs are commonly prescribed to relieve pain associated with osteoarthritis. These medications work by blocking enzymes responsible for the production of prostaglandins, chemicals that trigger inflammation and pain in damaged joints.
The different types of anti-inflammatories
NSAIDs (non-steroidal anti-inflammatory drugs)
These medications, such as ibuprofen, aspirin or naproxen, are the most commonly used to treat osteoarthritis pain. They block the COX-1 and COX-2 enzymes, which are responsible for the production of prostaglandins. However, by inhibiting COX-1, they can cause side effects such as gastric ulcers, kidney problems or even high blood pressure.
Paracetamol
Unlike NSAIDs, paracetamol does not have an anti-inflammatory effect, but acts as a pure analgesic. Although it is generally well tolerated, its use in high doses (more than 4g/day) can cause liver damage.
Selective COX-2 inhibitors (anti-COX2)
These drugs, such as celecoxib, were developed to target only the COX-2 enzymes responsible for inflammation, without affecting COX-1. They therefore offer less risk of gastrointestinal side effects. However, they are associated with an increased risk of cardiovascular complications.
The limits of anti-inflammatories
Although anti-inflammatory drugs provide effective and rapid relief, they only treat the symptoms and not the underlying cause of osteoarthritis. In addition, their prolonged use is often accompanied by risks:
- Digestive side effects: including ulcers, gastric bleeding and acid reflux.
- Kidney problems: NSAIDs can affect blood flow to the kidneys, leading to impaired kidney function.
- Cardiovascular risk: Selective COX-2 inhibitors may increase the risk of heart attacks and strokes.
In summary, anti-inflammatory drugs, although useful in the short term, cannot be considered a sustainable or safe solution, especially when taken over a long period of time.
The mechanism of inflammation in osteoarthritis
To understand why anti-inflammatory drugs are used for osteoarthritis, it is essential to understand the inflammatory process that accompanies this disease.
Inflammation is a natural reaction of the body to an aggression (infection, trauma, cartilage damage, etc.). When cartilage is damaged, it triggers a cascade of inflammatory reactions aimed at protecting the affected area. However, in the case of osteoarthritis, this inflammation becomes chronic and contributes to the progressive destruction of the cartilage.
The inflammatory process is mediated by cytokines, proteins such as IL-1B (interleukin-1B), which activate enzymes called COX-2. These enzymes then produce prostaglandins, molecules that amplify pain and inflammation in the affected joint.
Anti-inflammatory drugs work by blocking COX-2, which decreases the production of prostaglandins and reduces pain. However, they do not stop the breakdown of cartilage, which continues to worsen over time.
Below, a drawing provides an overview of the inflammatory process.

The action of COX enzymes: COX-1 vs COX-2
It is important to distinguish between COX-1 and COX-2:
- COX-1: These enzymes are present throughout the body and play a protective role, particularly by protecting the gastric mucosa and ensuring the proper functioning of the kidneys.
- COX-2: These enzymes are activated during inflammation. Their inhibition reduces pain but can also lead to adverse effects when not targeted correctly.
Why are anti-inflammatories not enough to treat osteoarthritis?
Osteoarthritis is not just inflammation; it is primarily a degenerative disease of the cartilage. While anti-inflammatory drugs can temporarily relieve pain, they cannot stop the degradation of cartilage.
The Role of Glucosamine and Chondroitin in Joint Health
Unlike anti-inflammatories, glucosamine and chondroitin are substances that occur naturally in cartilage and joints. They play a crucial role in maintaining the structure and function of cartilage. Several studies suggest that glucosamine may help slow the breakdown of cartilage, while chondroitin helps maintain the elasticity and hydration of cartilage.
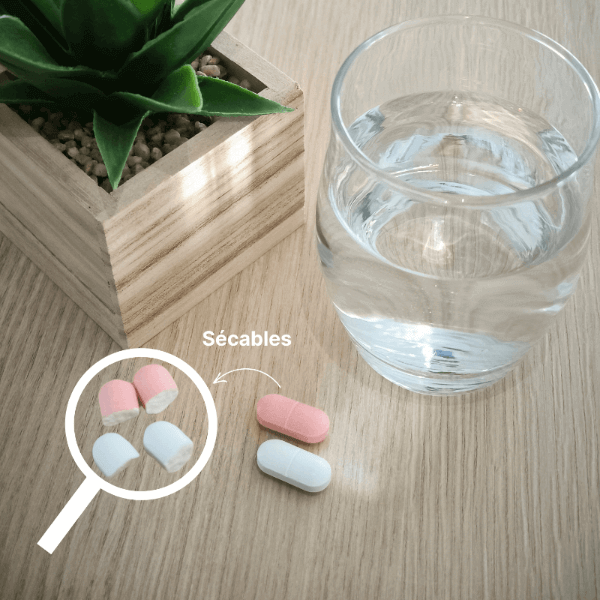
Dietary supplements that contain these two ingredients offer a natural solution to support joint health. Unlike anti-inflammatories, these substances aim to protect and strengthen cartilage, rather than simply masking pain.
Glucosamine: a gentler alternative to anti-inflammatories
Glucosamine, at a dose of 1500 mg, is a molecule that acts on both the structure of cartilage and on inflammatory mechanisms. Here are some reasons why glucosamine is an interesting alternative to classic anti-inflammatories:
- Action on cartilage: Glucosamine is a natural component of cartilage. It participates in the production of proteoglycans, molecules that allow cartilage to retain water and remain flexible. It also helps reduce cartilage degradation by inhibiting certain destructive enzymes.
- Modulation of inflammation: Although not an anti-inflammatory in the strict sense, glucosamine helps modulate inflammatory mediators involved in osteoarthritis, particularly IL-1B and the inflammatory cascade that activates COX-2 enzymes. Unlike conventional anti-inflammatories, it works without serious side effects on the stomach or kidneys, making it particularly interesting for long-term use.
- Long-term tolerance: Glucosamine is well tolerated over long periods of time. Unlike NSAIDs, which cannot be used continuously due to the risk of side effects, glucosamine can be taken regularly to help maintain joint health.
The preventive effect of Cartilamine
In addition to its role in managing the symptoms of osteoarthritis, Cartilamine can also be used preventively to protect joints, particularly in people who engage in regular physical activity or those who wish to prevent age-related joint wear and tear. By helping to maintain healthy cartilage, glucosamine and chondroitin help preserve mobility and reduce the risk of long-term joint degeneration.
Comparison between anti-inflammatories and glucosamine: when to use them?
The use of anti-inflammatory drugs can be useful in cases of acute inflammatory flare-ups, where the pain is particularly strong and disabling. However, their use must remain limited in time due to the health risks.
Conversely, glucosamine and chondroitin supplements are better suited for long-term use to help protect joints and support cartilage health. They do not cause the side effects of anti-inflammatories and work on the underlying cause of joint degradation, not just the pain.
Conclusion: A combined approach for the management of osteoarthritis
In conclusion, although anti-inflammatory drugs play a crucial role in the short-term relief of osteoarthritis pain, they are not a permanent solution. Their use should be cautious and limited in time due to potential side effects, particularly on the digestive system, kidneys and heart. In the long term, gentler and more natural solutions such as glucosamine and chondroitin, present in food supplements such as Cartilamine, can offer significant support in maintaining joint health and slowing the progression of osteoarthritis.







5 comments
Aucun effet bénéfique après prise de la glucosamine. Seule la chondroïtine au début de mon arthrose a permis un réel soulagement.
J’au de l’arthrose aux épaules avec des douleurs chroniques srtout la nuit qui m’empeche de dormir. je vais essayer la glucosamine et la chondroïtine. Je verrais.
Je souffre énormément de crises d’arthrose.
L’humidité de ma région y est certes une cause,mais je ne sais plus quoi faire, cette situation devient très invalidante.
Je souffre tellement j’ai une prothèse droite mais maintenant la gauche me. Fait mal j’ai donc les 2 genoux très douloureux
Merci pour ces renseignements . Où peut-on se procurer ces compléments dont vous parler svp ? Remerciements